With a burden of more than 1.2 million persons diagnosed with malignant diseases and over 0.7 million associated deaths in India per year, cancer remains a major public health problem.
Many cancer deaths are avoidable because of inadequate cancer prevention, screening, recovery, or survivorship care. Simultaneously, cancer care spending is high and increasing, placing a burden on national and private health insurance programs and family budgets. One of the most critical problems in India is ensuring that cancer care is affordable and accessible across all communities. To promote the reduction in cancer mortality, these issues must be addressed in the context of health care delivery.
Prevention begins with awareness
Awareness promotes self-identification and assessment of behaviors that may lead to cancer and ways to reduce one’s risk. Modifiable lifestyle behaviors such as smoking, poor diet, and lack of physical exercise contribute to the development of certain forms of cancer. Since these patterns frequently arise during the formative stages of life, it is particularly important to begin early in educating about healthy living. Public health programs aimed at enhancing nutritious diet, improved plans with provisions for space to exercise, and obesity reduction in India’s population will also help to delay the rise in lifestyle-related cancers.
Apart from creating awareness, community workers and volunteers can be trained to perform door-to-door visual examinations of oral cavities among high-risk people. With additional remuneration, they can also obtain self-collected samples from women who are unwilling for cervical cancer screening and transport them to the HPV testing centers.
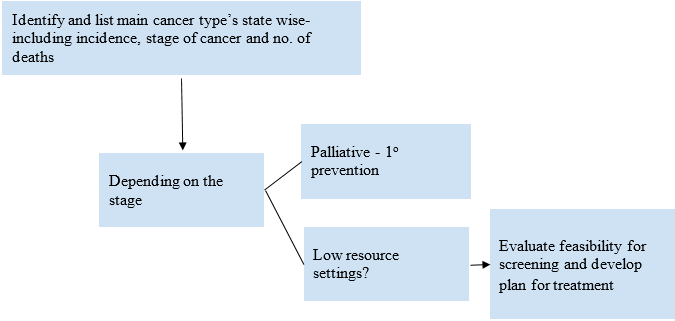
Key control strategies for reducing the cancer burden in India
One of the primary causes for the disparity in cancer outcomes between high-income and lower-middle-income countries is the significant delay in cancer screening and diagnosis in lower-middle-income countries. Early detection detects cancer at an early stage when it has a high chance of being cured. An early detection program should consist of the following activities: screening, diagnosis, treatment, and follow-up.
Screening should be both effective and opportunistic. An effective screening means it can be applied to over 70% of the population at risk. For example, cancers of the oral cavity and lungs account for more than 25% of cancer deaths in men, while cancers of the breast and cervix account for 25% of cancer deaths in women. Oral cancer screening should focus on the high-risk groups based on their habits- such as those who consume tobacco products, alcohol, betel nut, or paan. Since tobacco users are considered a high-risk group for NCDs, it also offers an opportunity to screen them for multiple diseases in the same setting.
The cost burden of cancer care
A cost-effective approach to population-based screening should be established, along with potential methods for obtaining the necessary resources from both governmental and non-governmental sources.
According to the data released by the Atomic Energy Regulatory Board, only 11% of the radiotherapy facilities are available to the eastern region of India, which constitutes about 26% of the Indian population. Cancer surgery and radiotherapy are inequitably available in metropolitan areas, and radiotherapy is severely under-resourced (Mallath et al., 2014). Addressing the social determinants of cancer and cancer-related needs must coexist with increased cancer treatment capacity and delivery capabilities in India.
The need for a political will
Several measures such as commitment to limit, and eventually eliminate the use of tobacco products by vigorous enforcement of the Framework Convention on Tobacco Control will, over time, significantly reduce the prevalence, and thereby mortality caused by, many common types of cancer in India.
Identification of gaps for more effective prevention and improved outcomes
The focus of assessing the existing early detection strategy and other programs should be on the gap between what is expected and what is available, such as how well structured the current cancer detection programs are, what percentage of people are covered, or how often people are screened. This can be done by a detailed profiling state-wise to identify the critical gaps and addressing them by prioritizing research.
About the Author:
Dr. Demi Miriam
Dr. Demi Miriam is the Technical Lead – Public Health at CHD Group India Country Office.
Disclaimer: Views expressed are the author’s own. CHD Group takes no liability on behalf or for the contents expressed.


